Scheduling eye exams regularly is an integral part of keeping your eyes healthy. A comprehensive eye exam does much more than update your prescription.
It also checks your eyes for any signs of eye conditions. Eye conditions are especially prevalent in adults over 40, as the most common eye conditions are age-related.
One of the most common of these is glaucoma. The best way to screen for glaucoma is through tonometry. Tonometry is tested when you have an eye exam.
Tonometry tests your eye pressure. Keep reading to learn more about tonometry and why testing it is an essential part of any eye exam!
What is Eye Pressure, and Why is it Necessary?
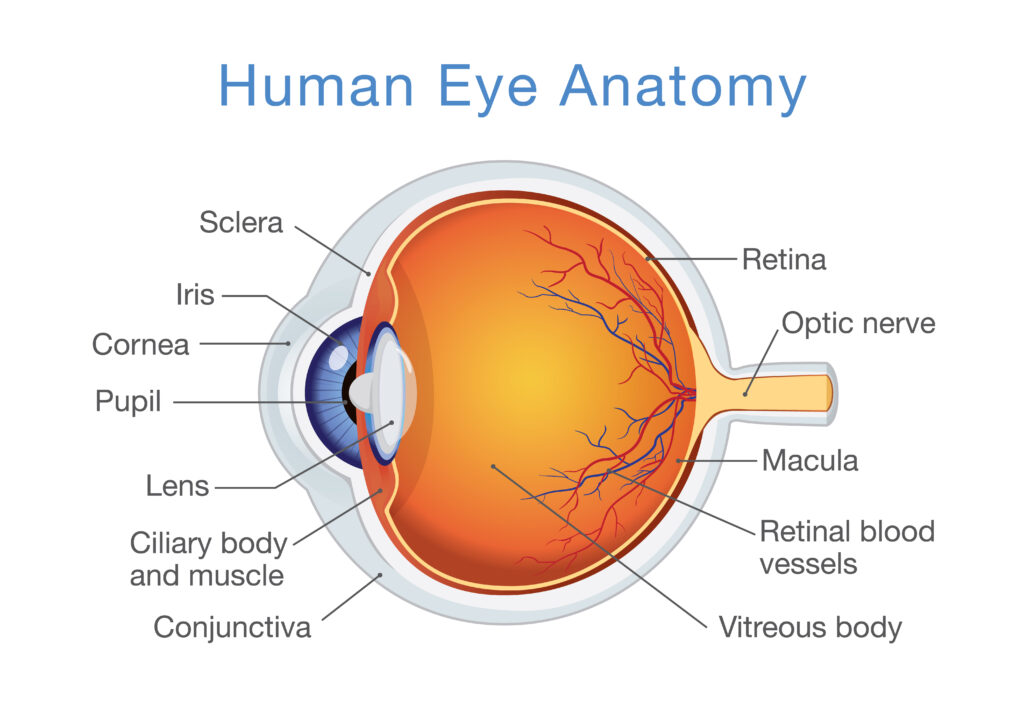
Your eyes are filled with fluid. This fluid, called the aqueous humor, constantly flows in and out of your eye.
The flow of aqueous humor keeps your eyes healthy by supplying nutrients to different parts of the eye. It also inflates the cornea to protect against foreign contaminants like dust and harmful bacteria.
Aqueous humor must be produced and drained from the eye at an equal rate. Doing this helps maintain a healthy eye pressure called intraocular pressure, or IOP.
But sometimes, the fluid in the eye doesn’t drain at the same rate it’s being produced. Most of the time, when this happens, IOP increases as fluid builds up in the eye.
High intraocular pressure can have severe consequences on how healthy your eyes are. In most cases, it can lead to glaucoma or even total loss of vision. The best way to measure IOP and make sure it isn’t elevated is through tonometry.
What is Tonometry?
Tonometry measures your intraocular pressure. Even if you’re young, most eye doctors use tonometry during your eye exam. It’s imperative to catch high intraocular pressure levels as early as possible to prevent vision loss from glaucoma.
Tonometry is also a simple test, so it takes little time to perform. But before talking about how tonometry is performed during an eye exam, it’s crucial to understand why eye doctors use tonometry.
Glaucoma and Tonometry
Glaucoma is one of the leading causes of blindness in adults over 60. It’s often called the “Silent Thief of Sight” because it doesn’t show any symptoms in the early stages of the eye condition.
Most patients with glaucoma don’t realize they have it until irreversible vision loss has already occurred. By the time it causes visual symptoms, they are irreversible.
Any vision lost as a result of glaucoma is permanent. Glaucoma damages the optic nerve, which connects your eye to your brain.

When damaged, your optic nerve can no longer correctly relay what you see to your brain, so you only get an incomplete picture. Glaucoma affects your peripheral vision first, and as it worsens, you’ll begin to experience tunnel vision. Eventually, you can go completely blind.
There are several kinds of glaucoma. A buildup of eye pressure causes the most common types of glaucoma.
Having too much intraocular pressure strains the optic nerve and causes damage to it over time. The first sign of glaucoma is having elevated intraocular pressure, which you can’t feel.
However, your eye doctor can diagnose increased or elevated intraocular pressure with tonometry. Ideally, your eye doctor will see that you have high IOP before you can develop glaucoma.
That means you can receive preventative treatment to prevent damage to the optic nerve and delay the development of glaucoma. This is usually done by taking eye drops that lower IOP.
Early intervention can stop glaucoma from damaging your vision and slow its progression. Tonometry can save your vision.
There’s no reason to wait until you experience glaucoma symptoms or think you have glaucoma to see an eye doctor. Have eye exams regularly to get tonometry, helping to detect glaucoma long before you have any vision loss!
How Tonometry Works

There are three main ways tonometry is performed. One is a contact method that uses a slit lamp. Numbing eye drops, along with a dye, are first applied to your eyes.
Then your eye doctor uses the slit lamp, which has a place to hold your head at the chin and forehead, while a tonometer barely touches your eye. The dye in your eye changes colors to indicate your IOP.
The contact method of tonometry can also be performed with a hand-held device that touches the eye and instantly reads your IOP. There’s also a non-contact tonometry method that uses a quick puff of air to flatten the cornea.
A beam of light is centered on the eye along with the puff of air to detect how much the cornea flattens, which helps determine your intraocular pressure. All these methods are quick, painless, and can potentially save your vision!
Normal Eye Pressure Ranges
Your intraocular pressure is measured in the same units as your blood pressure, which is mmHg or millimeters of mercury. The ideal range for IOP is 10-21 mmHg. If your intraocular pressure is higher, it can be because you already have glaucoma or you will develop it.
It’s rarer for your IOP to be below this range, but it can happen. Low intraocular pressure may mean you have a condition known as hypotony. Hypotony can cause vision loss, so like glaucoma, it also requires early intervention and treatment.
No matter what your IOP is, it’s important to have it measured regularly. The only way to have it routinely measured is by having eye exams on a regular basis with your eye doctor. So make sure you have an eye exam at least once every two years, especially by the time you turn 40!
Do you need to schedule an eye exam? Schedule yours at Sugiki Portis Yim Eye Center in Honolulu, HI, today, and keep your eyes happy and healthy!